Tools of the Trade - Intravenous Catheter
- Category: Treatment
- Posted On:

How Pig Bladders, Cholera, and Plastic Changed Medicine
Joshua Strommen MD
Have you ever been so sick with vomiting and diarrhea that you needed intravenous (IV) fluids to help you feel better?
Have you been hospitalized and needed IV medicines to help fight infection, ease pain, give you blood, sustain your blood pressure, or treat the devastating effects of a stroke?
Have you ever had surgery or been given a stent to open arteries in your heart?
All these functions listed above are completely dependent on the techniques and ideas that mostly originated in the 17th century. The IV catheter has revolutionized modern medicine; however there have been many failures, deaths, and setbacks in honing this therapeutic intervention over the last 400 years.
A brief historical glimpse is needed to paint a complete picture of the journey this device has made.
.jpg)
In 1492 Pope Innocent VIII had a stroke, which left him severely disabled. A physician at the time had the idea of giving him blood from three healthy male boys to see if it would improve his morbid state. At that time, no IV as we know it was available, so the doctor connected the boys’ veins to the Pope’s veins, and unfortunately all four of them died. This led to about a hundred-year absence of any further attempts at intravenous intervention.


It wasn’t until 1658 when several English scientists began heavily experimenting with primitive IV catheters. The distinguished company of Oxford elite who began this charge included Robert Boyle (of ‘Boyle’s Law’), Thomas Willis (of ‘Circle of Willis’), John Locke (father of the Enlightenment movement), and Robert Hooke (of ‘Hooke’s Law’). They decided to use a feather quill and the bladder from a pig to create the first infusion device. This device infused a concoction of wine, ale, opium, and antimony (a metal that when combined with other chemicals was thought to cleanse the body) into a dog. The dog did well, shockingly. From this point many other infusions were made and given to animals for scientific study.
One big problem was blood clotting at the insertion site of the quill. Many different agents were tested to come up with another alternative for a conduit to infuse the desired liquid. For some time, silver was the agent of choice
In 1665 the first transfusion of blood from the blood of a mastiff dog into the jugular vein of another medium sized dog with no complications occurred. It was the first successful transfusion of blood from one living species to another.
On June 15, 1667 the first animal to human transfusion occurred. A man, who was mentally deranged, was given 9 ounces of blood from a lamb in an attempt to cure his mental illness. The idea of giving blood from a bashful sheep to a psychotic human endured for some time.

This man unfortunately had one of the first documented transfusion reactions where he became gravely ill after receiving the blood. There was no knowledge of blood typing at that time (this came along in 1901), and this was to their detriment because many other humans died in France and England from this lack of specific knowledge.
After another 100 years of banning blood transfusions, in 1795 Dr. Philip Physick, known as the American “Father of Modern Surgery” suggested human to human transfusions.

§ In 1818 a British obstetrician used the blood from a woman’s husband to transfuse into her as she was bleeding profusely after giving birth, a condition called post-partum hemorrhage. This was the first successful human-to-human blood transfusion. Unfortunately post partum hemorrhage is still the leading cause of mortality in the world for post partum moms.
1832 was the year where Cholera spread to Western Europe. It was a devastating disease where scientists noted that the blood of those infected was very concentrated due to the water loss from their diarrhea. Consequently, the first infusion of ‘Normal Saline’ was performed and it successfully treated numerous patients dying from dehydration.
The 1840’s and 1850’s brought further refinement of the metal needle and the glass syringe due to an intense need for treatment of dehydration due to Cholera’s deadly grip on humanity.
100 years later in the 1950’s, plastics, and more specifically PVC, became the ingredient of choice when constructing IV catheters. Plastic at that time also replaced rubber tubing and glass bottles, which transported the fluid and stored the fluid respectively.
Since the 1950’s, IV catheters have undergone significant changes to minimize vessel irritation, blood clots and infection. These changes include going from PVC, to Teflon, and now to polyurethane as the plastic of choice. The types of fluids infused underwent heavy study and scrutiny in the 19th and 20th century. Ironically, the debate still rages as of this day as to how best treat different conditions with the proper fluid. Shockingly, it wasn’t until the early 1970’s at Massachusetts General Hospital did nurses begin inserting IV catheters. Traditionally, it was a procedure performed by physicians only.
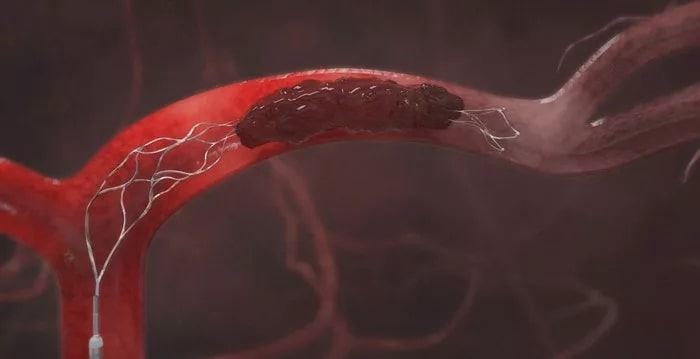
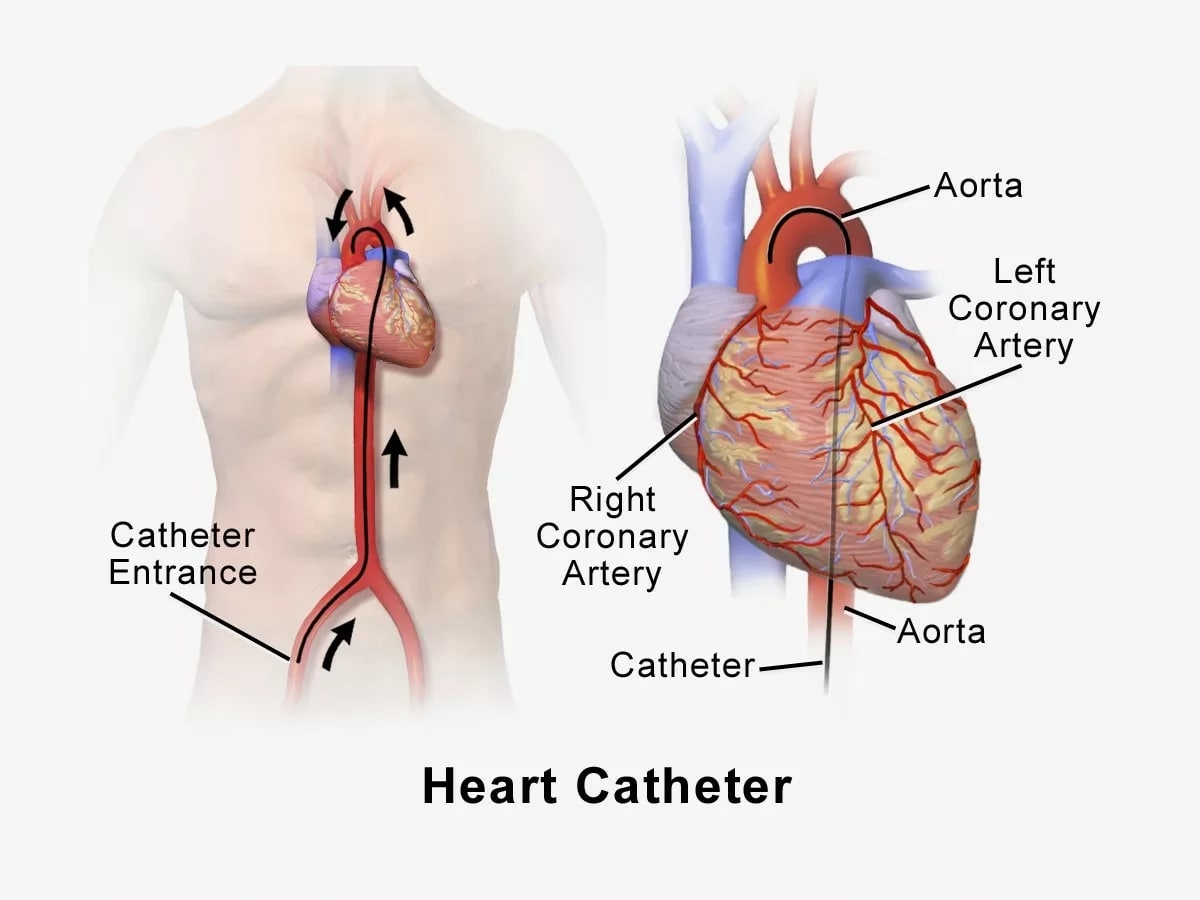
As you can see, the revolution has been remarkable. We have gone from a feather quill and pig bladder to polyurethane, antibacterial coated, preservative free plastic. We have traversed a time where giving blood to the pope without checking blood types was unknowingly attempted to now having about a 1% incidence of a serious reaction due to blood transfusions. Due to the development of needles and plastic, we went from being able to hydrate a patient with cholera to being able to insert a wire that goes from your groin all the way into your heart where a device is placed to open a coronary artery, which improves the likelihood of surviving from a major heart attack. We can even insert a catheter into the arteries of your brain and remove a blood clot that is causing a stroke. The transformation has been no less than miraculous, and it seems to still be improving as we move forward.

Joshua Strommen is an Emergency Medicine Physician at Premier ER & Urgent Care. He graduated from the University of Texas at Houston Medical School in 2010. Subsequently, he was in the US Army for 6 years, where he had the opportunity to serve as an Attending Physician and also an Assistant Program Director for the Emergency Medicine residency program at Carl R Darnall Army Medical Center in Ft. Hood, TX.
